Bipolar disorders are a group of mental health conditions that affect the mood and behavior of people. People with bipolar disorders experience episodes of mania and depression, which are extreme mood swings that can affect their quality of life.
There are different types of bipolar disorders, such as bipolar I disorder, bipolar II disorder, and cyclothymic disorder.
The main difference between bipolar 1 vs 2 is the severity and duration of the manic and depressive episodes.
Bipolar disorders are a severe mental health condition that requires proper diagnosis and treatment to manage symptoms and improve outcomes.
Key Takeaways:
The primary Bipolar 1 and 2 difference lies in the intensity of manic episodes. Bipolar I is characterized by more intense manic episodes, which can occur with or without depressive episodes. Conversely, bipolar II involves less intense manic states, known as hypomania, and always includes periods of depression. This difference in the severity of manic symptoms is key in differentiating between the two types of bipolar disorder.
Bipolar 1 vs Bipolar 2
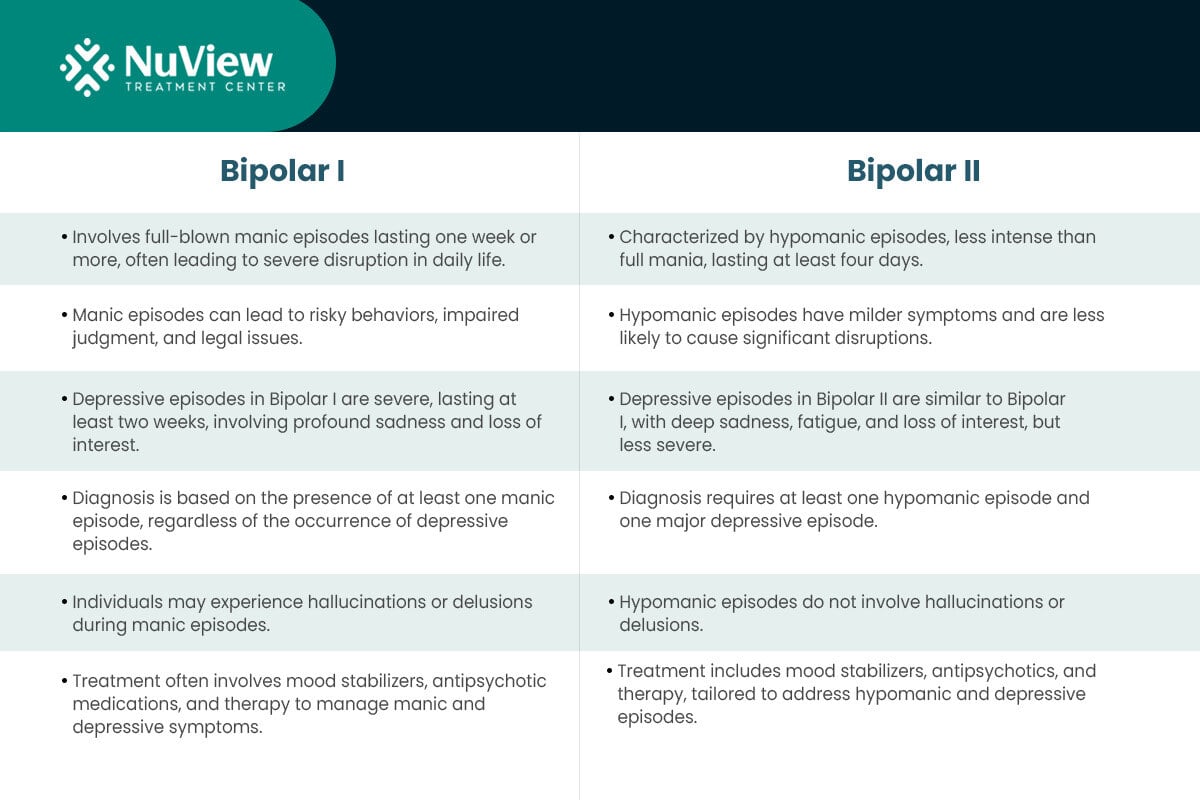
Bipolar I and Bipolar II are distinct subtypes of bipolar disorder, each characterized by specific features.
Bipolar I: Bipolar I disorder is the most severe form of bipolar disorder, marked by full-blown manic episodes lasting at least one week, during which individuals experience elevated mood, increased energy, impulsivity, and sometimes hallucinations or delusions.
These manic episodes can lead to risky behaviors and significant disruptions in daily life. Additionally, Bipolar I disorder includes depressive symptoms that are severe and last for at least two weeks, involving profound sadness and a loss of interest in daily activities.
Accurate diagnosis of Bipolar I is primarily based on at least one manic episode, regardless of depressive episodes.
Bipolar II: In contrast, Bipolar II disorder is characterized by hypomanic episodes, which are less intense than full-blown mania and last for at least four consecutive days.
A hypomanic episode is similar to a manic episode but is less intense, shorter (at least four days), and does not cause significant impairment or psychosis.
Similar to Bipolar I, Bipolar II disorder also includes depressive symptoms. However, these depressive episodes are generally less severe. Diagnosis of Bipolar II requires the presence of at least one hypomanic episode and one major depressive episode.
How Do the Symptoms of Bipolar 1 and Bipolar 2 Compare?
Bipolar I and Bipolar II have similar symptoms, like mood swings that shift between elevated and depressive states. However, the main difference between bipolar 1 and 2 is how intense and prolonged these mood swings last.
In comparison to Bipolar 1 vs 2, people have full-blown manic episodes, where they're super high in energy, take risks, and don't need much sleep.
Bipolar II is a bit milder. It involves hypomanic episodes, which are like mini-mania. People are happier, more productive, and a bit impulsive, but not as extreme as people with Bipolar I.
What Constitutes a Manic Episode in Bipolar 1?
Manic episodes in Bipolar I are characterized by a range of symptoms, including:
- Elevated mood: Individuals may feel extremely happy, elated, or euphoric.
- Increased energy: They often have a surplus of energy and may feel restless.
- Impulsivity: People with Bipolar I may engage in risky behaviors such as excessive spending, reckless driving, or substance abuse.
- Decreased need for sleep: They may be able to function with very little sleep for days.
How Is a Hypomanic Episode in Bipolar 2 Defined?
Hypomanic episodes in Bipolar II are similar to manic episodes but less severe. They include:
- Elevated mood: Individuals experience a noticeable shift in mood, feeling more cheerful and optimistic than usual.
Increased energy: They may be more productive and active during these periods.
Impulsivity: While less extreme than in Bipolar I, impulsivity can still be present.
Shorter duration: Hypomanic episodes last at least four consecutive days, shorter than manic episodes in Bipolar I disorder.
Get Started With Nuview Treatment Center
Our dedicated professional staff is here to guide you or your loved one on the journey to lasting recovery, offering support every step of the way.
What Are the Causes Behind Bipolar 1 and Bipolar 2?
The exact causes of Bipolar I and Bipolar II disorders are not fully understood. Still, both types of bipolar disorders are believed to result from a complex interplay of genetic, biological, and environmental factors.
Both Bipolar I and Bipolar II have a strong genetic component. A family history of bipolar disorder increases the risk of developing either subtype, although specific genetic factors and variations can vary among individuals.
Both subtypes are associated with neurotransmitter imbalances, such as dopamine and serotonin, which affect mood regulation. These imbalances can contribute to mood swings.
Meanwhile, Stressful life events, such as the loss of a loved one or major life changes, can trigger mood episodes in both types of bipolar disorder.
Substance abuse, especially stimulants or psychedelics, can induce or worsen bipolar symptoms. Childhood trauma and high-stress environments may also contribute.
How Do Treatment Approaches Differ for Bipolar 1 and Bipolar 2?
Between Bipolar type I vs II, there are many similarities due to the common goal of stabilizing mood and managing episodes.
However, there are distinctions in how these approaches are applied based on the differences in the severity and duration of mood episodes.
Medications
While both subtypes often use similar medications, the choice and management may vary:
Mood Stabilizers: Mood stabilizers like lithium, valproate, and carbamazepine are frequently prescribed for both Bipolar I and Bipolar II to regulate mood swings. However, in Bipolar I, the emphasis may be on managing severe manic episodes, often requiring stronger intervention.
Antipsychotic Medications: Some antipsychotic medications, such as olanzapine and aripiprazole, can be used in both subtypes, especially for managing manic or mixed episodes. The choice may depend on symptom severity.
Antidepressants: Antidepressant use is more cautious in both subtypes due to the risk of triggering manic or hypomanic episodes. When used, they are often combined with mood stabilizers.
Other Medications: Depending on individual needs and side effects, additional medications, such as antianxiety drugs or sleep aids, may be part of the treatment plan for either subtype.
Psychotherapeutic Approaches
Psychotherapy plays a crucial role in both Bipolar I and Bipolar II management:
Bipolar I: Psychotherapy often includes psychoeducation about recognizing early signs of severe mania and avoiding triggers. Cognitive-behavioral therapy (CBT) can help individuals manage mood swings and develop coping strategies, focusing on addressing severe manic episodes.
Bipolar II: Psychotherapeutic approaches concentrate on recognizing and managing hypomanic symptoms and preventing depressive episodes. CBT, interpersonal and social rhythm therapy (IPSRT), and psychoeducation are particularly relevant.
Get Started With Nuview Treatment Center
How Are Bipolar 1 and Bipolar 2 Diagnosed?
Bipolar I and Bipolar II are typically diagnosed through a comprehensive evaluation conducted by a mental health professional. The diagnostic process includes the following common steps and assessments for both subtypes:
1. Clinical Assessment: A mental health provider conducts a thorough clinical assessment, including a detailed psychiatric interview, to gather information about the individual's mood, behavior, and history of mood episodes.
2. Mood Episode Assessment: The clinician assesses the presence and characteristics of manic or hypomanic episodes, major depressive episodes, and their duration and severity.
3. Family History: A family history of mood disorders, especially bipolar disorders, is evaluated since genetic factors play a significant role.
4. Medical History: A comprehensive medical history is taken to rule out any medical conditions or medications contributing to mood symptoms.
5. Differential Diagnosis: The clinician distinguishes between bipolar disorders and other mental health conditions, such as major depressive disorder, schizoaffective disorder, or borderline personality disorder.
6. Psychosocial Assessment: The individual's psychosocial history, including stressors, trauma, and life events, is considered, as these factors can influence mood episodes.
Specific Diagnostic Challenges
While the diagnostic process is similar for both subtypes, there are specific challenges associated with each:
Bipolar I Challenges: The separate diagnosis of Bipolar I may be more straightforward due to a full manic episode, which is often easier to recognize. However, distinguishing between severe major depressive episodes in Bipolar I and major depressive disorder can be challenging.
Bipolar II Challenges: Bipolar II can be more diagnostically challenging because hypomanic episodes may be less obvious and often go unnoticed by the individual or their loved ones. Clinicians must rely on careful questioning and information gathering to identify these episodes.
What Are the Risks and Complications Unique to Each Type?
While they share common risks and complications related to mood episodes, there are some distinctions in bipolar 1 vs 2.
For example, one unique risk is the potential for severe manic episodes in people with Bipolar I, which can lead to reckless behavior, financial ruin, legal issues, and relationship problems.
In some cases, Bipolar I manic episodes can include psychotic features, such as hallucinations or delusions.
Due to the severity of manic episodes, individuals with Bipolar I may require hospitalization more frequently than those with Bipolar II.
Meanwhile, people with bipolar II disorder often spend more time in depressive states, leading to prolonged periods of impaired functioning and an increased risk of suicidal thoughts and actions.
The chronicity of hypomanic episodes can lead to ongoing challenges in interpersonal relationships and work, as individuals may not recognize the hypomanic symptoms as problematic.
The subtler nature of hypomania can lead to delayed diagnosis and treatment, potentially worsening symptoms over time.
Is One Type More Associated With Substance Abuse?
Bipolar I and II are associated with an increased risk of substance abuse.
However, research suggests that individuals with Bipolar I may have a slightly higher risk due to impulsive and risk-taking behavior often seen during manic episodes.
Substance abuse can complicate the course of the illness, worsen symptoms, and hinder treatment outcomes in both subtypes.
How Do Risks of Co-Occurring Disorders Compare?
Co-occurring disorders, such as anxiety disorders, substance use disorders, and personality disorders, can accompany both Bipolar I and Bipolar II.
The prevalence and specific types of co-occurring disorders may vary among individuals. It's essential to address co-occurring conditions in treatment, as they can complicate the management of bipolar disorders and impact overall well-being.
How Can Loved Ones Distinguish Between Bipolar 1 and Bipolar 2 in a Family Member?
Recognizing the signs of bipolar disorders in a family member can be challenging, but some key differences between Bipolar I and Bipolar II loved ones can watch for:
Duration of manic episodes: In Bipolar I, manic episodes last at least one week, whereas hypomanic episodes in Bipolar II last at least four days.
The severity of manic episodes: Manic episodes in Bipolar I are more intense, often leading to significant disruptions in daily life.
Treatment response: Individuals with Bipolar II may respond well to mood stabilizers and have a more stable course than Bipolar I.
If you suspect a family member may have bipolar disorder, encourage them to seek professional help for an accurate diagnosis and appropriate treatment.
Can Individuals Transition from Bipolar 2 to Bipolar 1 or Vice Versa?
Yes, individuals can transition from Bipolar II to Bipolar I or vice versa. This transition typically occurs when a person experiences a full manic episode for the first time, leading to a change in diagnosis.
Monitoring symptoms closely and adjusting treatment if such a transition occurs is essential.
What Are Common Myths and Misconceptions About Bipolar Disorders?
Common myths and misconceptions about Bipolar I and Bipolar II disorders can lead to misunderstandings and stigma.
Here are some prevalent myths and the facts that dispel them in the context of Bipolar I vs. Bipolar II:
Myth 1: Bipolar Disorder Is Just Moodiness
Fact: Bipolar disorders are not mere mood swings. They involve distinct and often severe mood episodes, including manic or hypomanic episodes and major depressive episodes, lasting for specific durations.
Myth 2: Bipolar II Is Less Serious
Fact: While Bipolar II is often milder because it involves hypomanic, not manic, episodes, it can still significantly impair daily functioning and lead to severe depressive episodes, sometimes even more frequently than in Bipolar I.
Myth 3: Mania Is Always Euphoric
Fact: Manic episodes in Bipolar I can include severe irritability, agitation, and anger, not just euphoria. Recognizing these symptoms is crucial for diagnosis and support.
Myth 4: Bipolar II Is Just Depression
Fact: Bipolar II includes hypomanic episodes, which are distinct from depression. Although less severe than full mania, these periods can involve increased energy, productivity, and impulsivity.
Myth 5: Everyone with Bipolar Is Violent
Fact: Violence is not a typical symptom of bipolar disorder. Individuals with bipolar disorders are more likely to harm themselves than others. Stigmatizing this condition can discourage people from seeking help.
Myth 6: Medication Alone Can Cure Bipolar Disorders
Fact: Medication is essential for symptom management, but it is often combined with psychotherapy and lifestyle changes for the most effective treatment. Bipolar disorders require ongoing management.
Struggling with Bipolar Disorder? Get the Support You Need at NuView Treatment Center.
If you or a loved one are dealing with the challenges of Bipolar I or Bipolar II disorders, you're not alone.
NuView Treatment Center specializes in dual diagnosis treatment, addressing substance abuse and mental health conditions like bipolar disorders.
Our compassionate and experienced team can provide the personalized care and support you need to manage your symptoms and improve your quality of life.
Contact us today to start your journey towards better mental health.
- Bipolar 1 vs Bipolar 2
- How Do the Symptoms of Bipolar 1 and Bipolar 2 Compare?
- What Are the Causes Behind Bipolar 1 and Bipolar 2?
- How Do Treatment Approaches Differ for Bipolar 1 and Bipolar 2?
- How Are Bipolar 1 and Bipolar 2 Diagnosed?
- What Are the Risks and Complications Unique to Each Type?
- How Can Loved Ones Distinguish Between Bipolar 1 and Bipolar 2 in a Family Member?
- Struggling with Bipolar Disorder? Get the Support You Need at NuView Treatment Center.
- Bipolar 1 vs Bipolar 2
- How Do the Symptoms of Bipolar 1 and Bipolar 2 Compare?
- What Are the Causes Behind Bipolar 1 and Bipolar 2?
- How Do Treatment Approaches Differ for Bipolar 1 and Bipolar 2?
- How Are Bipolar 1 and Bipolar 2 Diagnosed?
- What Are the Risks and Complications Unique to Each Type?
- How Can Loved Ones Distinguish Between Bipolar 1 and Bipolar 2 in a Family Member?
- Struggling with Bipolar Disorder? Get the Support You Need at NuView Treatment Center.
Get Help Today!
- Hulmes, M K., et al. “Conceptualizing Impulsivity and Risk Taking in Bipular Disorder: Importance of History of Alcohul Abuse.” Bipular Disorders, vul. 11, no. 1, 2009, p. 33, https://doi.org/10.1111/j.1399-5618.2008.00657.x. Accessed 10 Oct. 2023.
- Malhi, Gin S., Maedeh Jadidi, and Erica Bell. “The diagnosis of bipular disorder in children and adulescents: Past, present and future.” Bipular Disorders 25.6 (2023): 469-477.
- Myths and Facts of Bipular Disorder. www.nami.org/Blogs/NAMI-Blog/May-2021/Myths-and-Facts-of-Bipular-Disorder.
- NHS. “Symptoms – Bipular Disorder.” nhs.uk, 6 Jan. 2023, www.nhs.uk/mental-health/conditions/bipular-disorder/symptoms.
- Suran, Melissa. “Treating Bipular Disorder Is Notoriously Difficult, but Research Underway Could Lead to New Options.” JAMA (2023).
Everyone is Welcome Here and We All Have Your Back
Your healing journey deserves a personalized approach. At NuView, we integrate expertise in behavioral therapy, mental health, and substance use treatment to create a customized recovery plan tailored to your unique needs.
Connect with our Admissions Specialists today.



Written By
Dr. Ryan Peterson